Device Carveouts
The table below shows the number of device carveout percentage rates. "Device carveouts" are rates with revenue code that are one of ('0275', '0276', '0277', '0278').
Data Dictionary:
- payer MRF: number of providers from payer MRFs
- hospital MRF: number of providers from hospital MRFs
- num_providers: number of providers either source
- num_providers_with_both: number of providers with both payer and hospital MRF rates
- num_validated: number of providers with validated rates
- pct_validated: percentage of providers with validated rates
As an example: 1181 providers have rates from both payer and hospital MRFs for Aetna, and 876 of those have validated rates.
"Validated" means that the percentage rate is within 10% of each other.
| payer_mrf | hospital_mrf | num_providers | num_providers_with_both | num_validated | pct_validated | |
|---|---|---|---|---|---|---|
| ('7', 'Aetna') | 3670 | 1780 | 4269 | 1181 | 876 | 0.741744 |
| ('76', 'Cigna') | 2885 | 1728 | 3984 | 612 | 449 | 0.73366 |
| ('522', 'Kaiser Permanente') | 3393 | 152 | 3404 | 140 | 35 | 0.25 |
| ('643', 'United Healthcare') | 1005 | 1873 | 2542 | 335 | 202 | 0.602985 |
| ('42', 'Anthem') | 1522 | 565 | 1907 | 153 | 109 | 0.712418 |
| ('49', 'Blue Cross Blue Shield of Michigan') | 222 | 32 | 241 | 13 | 6 | 0.461538 |
| ('169', 'Blue Cross Blue Shield of Texas') | 0 | 239 | 239 | 0 | 0 | nan |
| ('50', 'Blue Cross Blue Shield of Minnesota') | 221 | 66 | 227 | 60 | 42 | 0.7 |
| ('390', 'Blue Cross Blue Shield of Kansas') | 197 | 36 | 210 | 23 | 17 | 0.73913 |
| ('461', 'Wellmark Blue Cross Blue Shield') | 196 | 52 | 208 | 11 | 11 | 1 |
| ('61', 'Regence Blue Cross Blue Shield') | 173 | 0 | 173 | 0 | 0 | nan |
| ('799', 'Quartz') | 164 | 36 | 169 | 31 | 30 | 0.967742 |
| ('403', 'Blue Shield of California') | 89 | 79 | 151 | 17 | 8 | 0.470588 |
| ('229', 'Blue Cross Blue Shield of New Jersey (Horizon)') | 98 | 64 | 150 | 6 | 5 | 0.833333 |
| ('388', 'Blue Cross Blue Shield of Florida (Florida Blue)') | 0 | 132 | 132 | 0 | 0 | nan |
| ('398', 'Blue Cross Blue Shield of Tennessee') | 81 | 66 | 125 | 22 | 15 | 0.681818 |
| ('389', 'Blue Cross Blue Shield of Illinois') | 0 | 102 | 102 | 0 | 0 | nan |
| ('391', 'Blue Cross Blue Shield of Louisiana') | 78 | 39 | 101 | 16 | 8 | 0.5 |
| ('300', 'Providence Health Plan') | 83 | 21 | 88 | 16 | 16 | 1 |
| ('52', 'Blue Cross Blue Shield of North Carolina') | 40 | 61 | 75 | 26 | 22 | 0.846154 |
| ('354', 'UPMC Health Plan') | 0 | 64 | 64 | 0 | 0 | nan |
| ('770', 'Mass General Brigham Health Plan') | 62 | 0 | 62 | 0 | 0 | nan |
| ('455', 'Blue Cross Blue Shield of Hawaii') | 57 | 0 | 57 | 0 | 0 | nan |
| ('628', 'Premera Blue Cross') | 23 | 35 | 54 | 0 | 0 | nan |
| ('299', 'Priority Health') | 7 | 49 | 50 | 6 | 2 | 0.333333 |
| ('286', 'MVP Health Care') | 0 | 50 | 50 | 0 | 0 | nan |
| ('720', 'Harvard Pilgrim') | 0 | 50 | 50 | 0 | 0 | nan |
| ('111', 'Geisinger') | 2 | 48 | 49 | 0 | 0 | nan |
| ('101', 'Blue Cross Blue Shield of New York (Excellus)') | 26 | 17 | 43 | 0 | 0 | nan |
| ('174', 'Highmark Blue Cross Blue Shield') | 0 | 42 | 42 | 0 | 0 | nan |
| ('458', 'Blue Cross Blue Shield of North Dakota') | 37 | 7 | 39 | 5 | 2 | 0.4 |
| ('51', 'Blue Cross Blue Shield of Nebraska') | 0 | 38 | 38 | 0 | 0 | nan |
| ('462', 'Blue Cross Blue Shield of Vermont') | 32 | 8 | 33 | 7 | 7 | 1 |
| ('317', 'Tufts Health Plan') | 0 | 33 | 33 | 0 | 0 | nan |
| ('636', 'SelectHealth') | 0 | 29 | 29 | 0 | 0 | nan |
| ('168', 'Blue Cross Blue Shield of South Carolina') | 19 | 16 | 28 | 7 | 4 | 0.571429 |
| ('383', 'Blue Cross of Idaho') | 5 | 23 | 26 | 2 | 2 | 1 |
| ('392', 'Blue Cross Blue Shield of Massachusetts') | 0 | 20 | 20 | 0 | 0 | nan |
| ('456', 'Blue Cross Blue Shield of Mississippi') | 14 | 6 | 19 | 1 | 1 | 1 |
| ('454', 'Blue Cross Blue Shield of Arkansas') | 0 | 15 | 15 | 0 | 0 | nan |
| ('166', 'Blue Cross Blue Shield of New Mexico') | 0 | 13 | 13 | 0 | 0 | nan |
| ('165', 'Blue Cross Blue Shield of Montana') | 0 | 11 | 11 | 0 | 0 | nan |
| ('56', 'Blue Cross Blue Shield of Pennsylvania (Independence)') | 0 | 10 | 10 | 0 | 0 | nan |
| ('44', 'Blue Cross Blue Shield of Maryland & DC (CareFirst)') | 0 | 8 | 8 | 0 | 0 | nan |
| ('53', 'Blue Cross Blue Shield of Oklahoma') | 0 | 7 | 7 | 0 | 0 | nan |
| ('43', 'Blue Cross Blue Shield of Arizona') | 0 | 7 | 7 | 0 | 0 | nan |
| ('723', 'Fidelis') | 0 | 5 | 5 | 0 | 0 | nan |
| ('160', 'Blue Cross Blue Shield of Alabama') | 0 | 5 | 5 | 0 | 0 | nan |
| ('397', 'Blue Cross Blue Shield of Rhode Island') | 0 | 3 | 3 | 0 | 0 | nan |
| ('54', 'Capital Blue Cross') | 0 | 1 | 1 | 0 | 0 | nan |
Code
Payer Device Rates SQL
WITH
network_spine AS (
SELECT
payer_id,
network_id,
network_name,
t.payer_data_network
FROM
tq_dev.internal_dev_csong_cld_v2_0_0.tmp_ref_network_spine_2025_05,
UNNEST(payer_data_network) AS t(payer_data_network)
),
payer_spine AS (
SELECT DISTINCT
payer_id,
payer_name
FROM tq_dev.internal_dev_csong_cld_v2_0_0.tmp_ref_payer_spine_2025_05
),
provider_spine AS (
SELECT
npi_value AS npi,
provider_id
FROM
tq_dev.internal_dev_csong_cld_v2_0_0.tmp_ref_provider_spine_2025_05,
UNNEST(npi) AS t(npi_value)
WHERE
provider_id IS NOT NULL
),
core_rates AS (
SELECT
cr.payer_id,
ps.payer_name,
ns.network_id,
ns.network_name,
ps.provider_id,
CASE
WHEN negotiated_rate < 1 THEN negotiated_rate * 100
WHEN negotiated_rate > 100 THEN NULL
ELSE negotiated_rate
END AS percentage
FROM tq_production.public_2025_05.core_rates cr
JOIN network_spine ns
ON ns.payer_id = cr.payer_id
AND ns.payer_data_network = cr.product_network_label
JOIN payer_spine ps
ON ps.payer_id = cr.payer_id
JOIN provider_spine ps
ON ps.npi = cr.provider_npi
WHERE billing_code_type = 'RC'
AND billing_code IN (
'0275',
'0276',
'0277',
'0278'
)
AND billing_class = 'institutional'
AND negotiated_type = 'percentage'
),
mode_rates AS (
SELECT
payer_id,
network_id,
provider_id,
percentage,
ROW_NUMBER() OVER (
PARTITION BY payer_id, network_id, provider_id
ORDER BY COUNT DESC
) AS rn
FROM (
SELECT
payer_id,
network_id,
provider_id,
percentage,
COUNT(*) as count
FROM core_rates
GROUP BY 1, 2, 3, 4
)
)
SELECT
cr.payer_id,
cr.payer_name,
cr.network_id,
cr.network_name,
cr.provider_id,
min(cr.percentage) as min_rate,
max(cr.percentage) as max_rate,
avg(cr.percentage) as avg_rate,
approx_percentile(cr.percentage, 0.5) as median_rate,
ANY_VALUE(mr.percentage) as mode_rate,
count(*) as num_rates
FROM core_rates cr
LEFT JOIN (SELECT * FROM mode_rates WHERE rn = 1) mr
ON mr.payer_id = cr.payer_id
AND mr.network_id = cr.network_id
AND mr.provider_id = cr.provider_id
GROUP BY 1, 2, 3, 4, 5
Provider Device Rates SQL
WITH
network_spine AS (
SELECT
payer_id,
network_id,
network_name,
t.payer_data_network
FROM
tq_dev.internal_dev_csong_cld_v2_0_0.tmp_ref_network_spine_2025_05,
UNNEST(payer_data_network) AS t(payer_data_network)
),
payer_spine AS (
SELECT
payer_id,
payer_name
FROM tq_dev.internal_dev_csong_cld_v2_0_0.tmp_ref_payer_spine_2025_05
),
provider_spine AS (
SELECT
npi_value AS npi,
provider_id
FROM
tq_dev.internal_dev_csong_cld_v2_0_0.tmp_ref_provider_spine_2025_05,
UNNEST(npi) AS t(npi_value)
WHERE
provider_id IS NOT NULL
),
hospital_rates AS (
SELECT
hr.payer_id,
ps.payer_name,
ns.network_id,
ns.network_name,
hr.provider_id,
CASE
WHEN negotiated_percentage < 1 THEN negotiated_percentage * 100
WHEN negotiated_percentage > 100 THEN NULL
ELSE negotiated_percentage
END AS percentage
FROM glue.hospital_data.hospital_rates hr
JOIN (
SELECT
DISTINCT
payer_id,
network_name,
t.plan_name
FROM tq_dev.internal_dev_csong_cld_v2_0_0.tmp_ref_plan_bridge_analysis_2025_05,
UNNEST(unique_plans) AS t(plan_name)
) pb
ON pb.payer_id = CAST(hr.payer_id AS VARCHAR)
AND pb.plan_name = hr.plan_name
JOIN network_spine ns
ON ns.payer_id = pb.payer_id
AND ns.network_name = pb.network_name
JOIN payer_spine ps
ON ps.payer_id = pb.payer_id
WHERE
LPAD(hr.revenue_code, 4, '0') IN (
'0275',
'0276',
'0277',
'0278'
)
AND hr.negotiated_percentage IS NOT NULL
AND contract_methodology = 'percent of total billed charges'
AND COALESCE(billing_class, '') != 'Professional'
AND payer_class_name = 'Commercial'
),
mode_rates AS (
SELECT
payer_id,
network_id,
provider_id,
percentage,
ROW_NUMBER() OVER (
PARTITION BY payer_id, network_id, provider_id
ORDER BY COUNT DESC
) AS rn
FROM (
SELECT
CAST(payer_id AS VARCHAR) as payer_id,
network_id,
provider_id,
percentage,
COUNT(*) as count
FROM hospital_rates
GROUP BY 1, 2, 3, 4
)
)
SELECT
CAST(hr.payer_id AS VARCHAR) AS payer_id,
hr.payer_name,
hr.network_id,
hr.network_name,
hr.provider_id,
min(hr.percentage) as min_rate,
max(hr.percentage) as max_rate,
avg(hr.percentage) as avg_rate,
approx_percentile(hr.percentage, 0.5) as median_rate,
ANY_VALUE(mr.percentage) as mode_rate,
count(*) as num_rates
FROM hospital_rates hr
LEFT JOIN (SELECT * FROM mode_rates WHERE rn = 1) mr
ON mr.payer_id = CAST(hr.payer_id AS VARCHAR)
AND mr.network_id = hr.network_id
AND mr.provider_id = hr.provider_id
GROUP BY 1, 2, 3,4, 5
Analysis
df = (
df_payer
.merge(
df_provider,
on=['payer_id', 'payer_name', 'network_id', 'provider_id'],
how='outer',
suffixes=('_payer', '_provider')
)
)
df
df['validated'] = (df['mode_rate_payer'] - df['mode_rate_provider']).abs() < 5
df['both_rates_present'] = df['mode_rate_payer'].notnull() & df['mode_rate_provider'].notnull()
df['payer_mrf'] = df['mode_rate_payer'].notnull()
df['hospital_mrf'] = df['mode_rate_provider'].notnull()
df_check = (
df
.loc[df['mode_rate_payer'].notnull() | df['mode_rate_provider'].notnull()]
.groupby(['payer_id', 'payer_name'])
.agg(
payer_mrf=('payer_mrf', lambda x: df.loc[x.index[x], 'provider_id'][x].nunique()),
hospital_mrf=('hospital_mrf', lambda x: df.loc[x.index[x], 'provider_id'][x].nunique()),
num_unq_providers=('provider_id', pd.Series.nunique),
num_providers_with_both=('both_rates_present', lambda x: df.loc[x.index[x], 'provider_id'][x].nunique()),
num_unq_providers_validated=('validated', lambda x: df.loc[x.index[x], 'provider_id'].nunique())
)
)
df_check = df_check.rename(columns={
'num_unq_providers_validated': 'num_validated',
'num_unq_providers': 'num_providers'
})
df_check['pct_validated'] = df_check['num_validated'] / df_check['num_providers_with_both']
df_check = df_check.sort_values('num_providers', ascending=False)
print(df_check.to_markdown())
More Details:
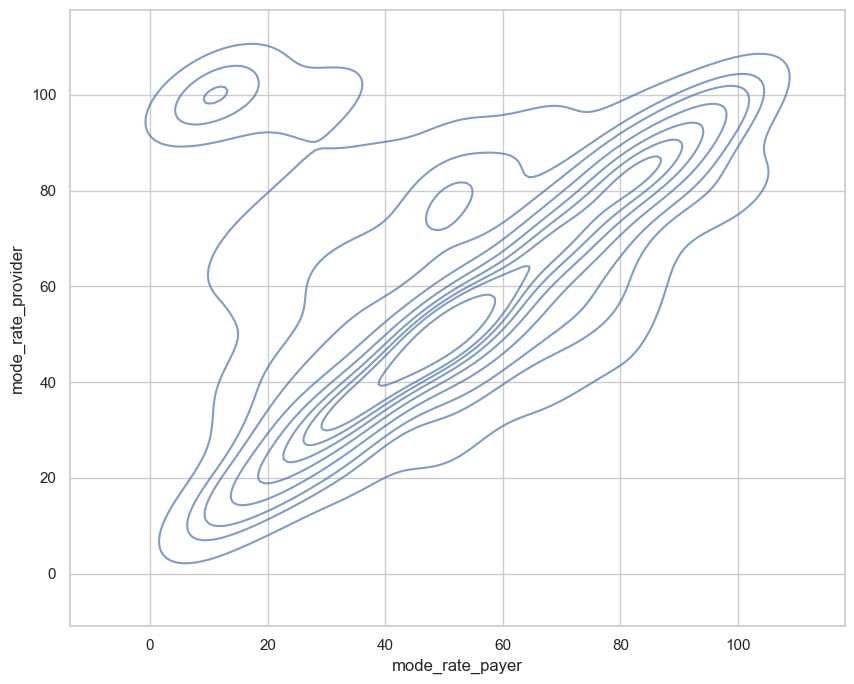
Density plot across all payers:
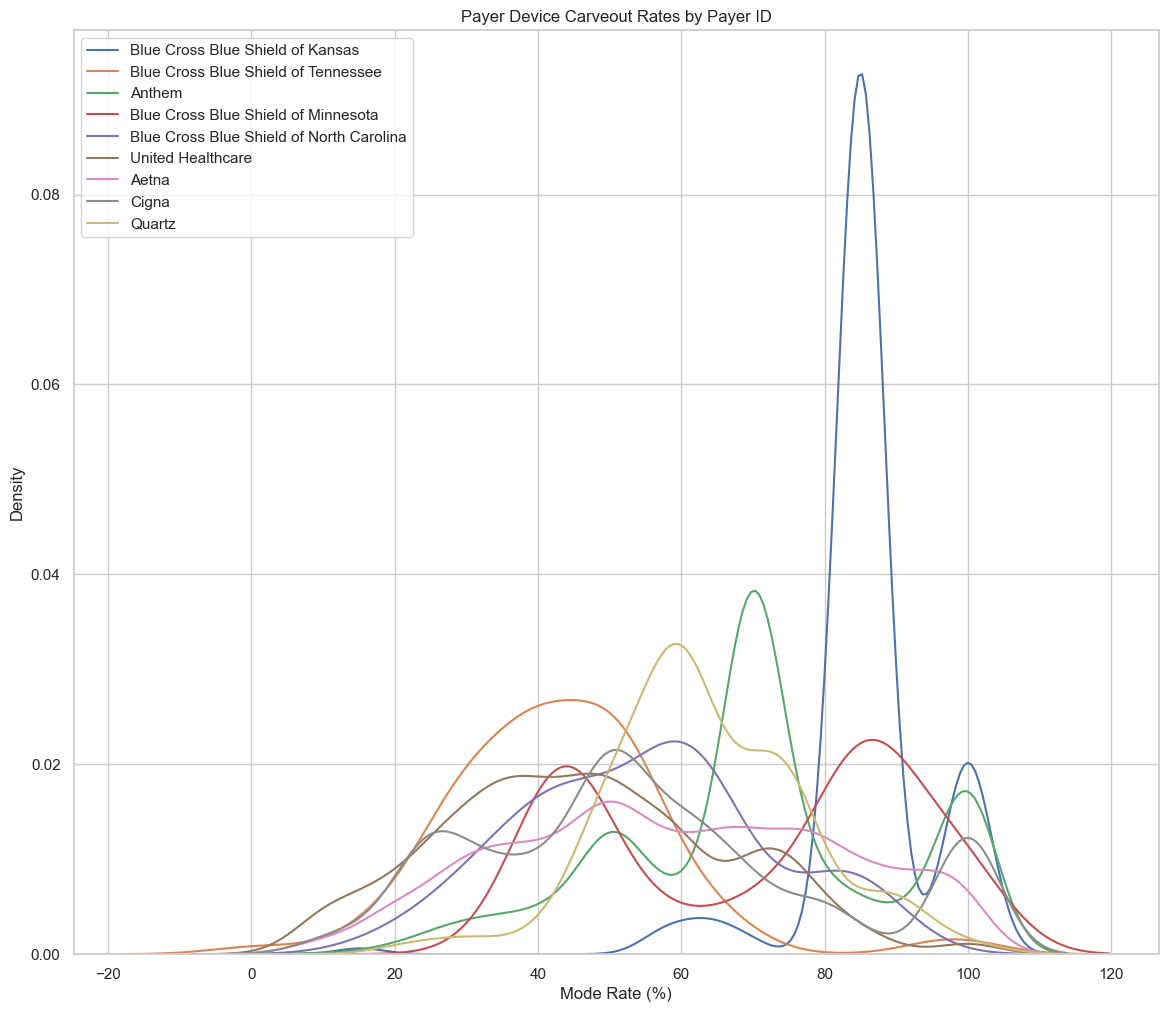
Distributions by payer: